- Статьи
- Science and technology
- Cellular calculation: a way has been found to improve the treatment of aggressive brain tumors
Cellular calculation: a way has been found to improve the treatment of aggressive brain tumors
Scientists have found a way to increase the effectiveness of a chemotherapeutic drug for the treatment of an aggressive type of brain tumor, glioblastoma, by activating several cell death pathways in the neoplasm. As part of the proposed approach, additional mechanisms are triggered, such as ultrasound, which stimulate the immune system against neoplasms. This will ensure an effective fight against drug-resistant cancer cells and the formation of immune control that prevents tumor recurrence, the scientists told Izvestia.
How to treat glioblastoma
Temozolomide (Temodal) is most often used as a chemotherapeutic agent for glioblastomas (aggressive brain tumors). It has a number of advantages, in particular, it overcomes the blood-brain barrier and penetrates into brain tissue, acting directly on tumor cells. In addition, the side effects of its action are well known and can be monitored in the clinic. However, for many patients, the effectiveness of such therapy is extremely low, since glioblastoma cells, due to a number of features, are able to "fight back" against the action of a chemotherapy drug and develop resistance to it.
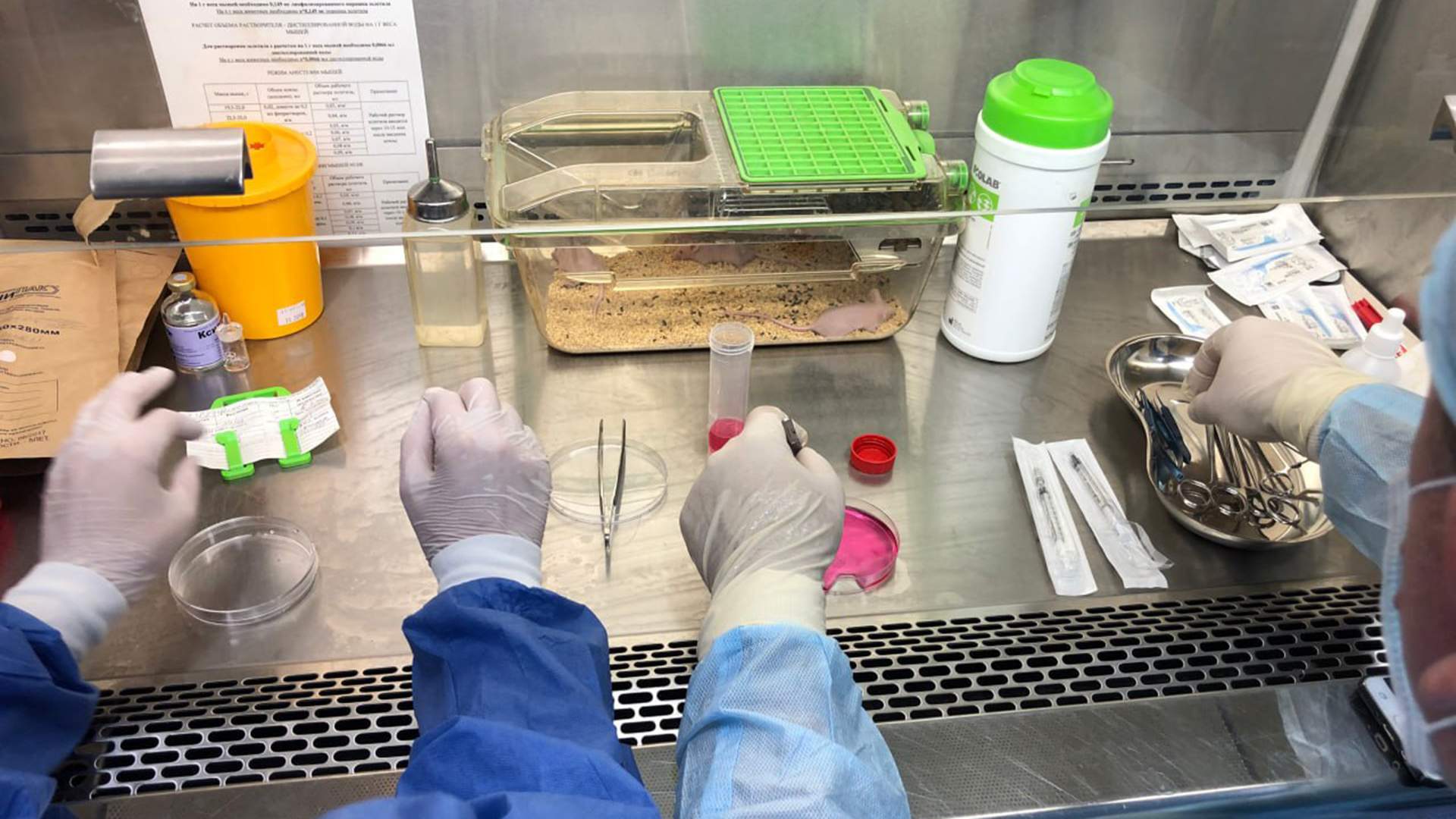
Scientists from the Institute of Biology and Biomedicine of the National Research Nizhny Novgorod State University (NNSU) named after N.I. Lobachevsky and Ghent University (Belgium) proposed to influence several ways of glioblastoma cell death, thus reducing the likelihood of their resistance to temozolomide. Launching several deadly cellular cascades will also potentially allow fighting functionally different cells inside the tumor. Researchers have already shown the possibility of this approach in a number of studies using animals as experimental models.
According to the proposed approach, in parallel with the launch of the classical mechanism of action of temozolomide, an alternative pathway of cell death is activated, which has immunogenic properties — it helps the immune system to become a participant in the fight against neoplasm. You can start it with the help of additional medications or some physical effects, such as ultrasound.
"Temozolomide is an attractive chemotherapeutic agent for the proposed combination therapy, which will improve the effectiveness and quality of treatment for patients with glioblastomas," Tatiana Mishchenko, project manager, Associate professor of the Department of Neurotechnology at the Institute of Biology and Biomedicine of the National Research University, told Izvestia.
Glioblastoma is a tumor that affects brain cells and is considered the most aggressive type of cancer. During its treatment, the patient has a neoplasm surgically removed, then radiation therapy is performed in combination with chemotherapy. The effect of these methods is mainly aimed at damaging the DNA of the remaining cancer cells, which leads to their death and reduces the risk of tumor re-growth.
How to launch an immunogenic pathway against tumors
When death is triggered by the immunogenic pathway, tumor cells release special "danger molecules" that attract specific cells of the immune system, dendritic cells, to the site of their death. These, in turn, absorb fragments of dying cells and "present (show) the dying enemy" to T-lymphocytes. Similar fragments are present in living cancer cells, which become targets for T-lymphocytes. As a result, a specific immune response is formed that destroys the glioblastoma cells that remain alive after therapy. In addition, the immune system then begins to closely monitor in order to prevent relapses.
The authors proposed using a combined approach using nanocarriers that would allow targeted delivery of temozolomide and other substances necessary to trigger immunogenic cell death to the tumor. Targeted delivery will reduce possible side effects on healthy human cells.
— In the future, we plan to evaluate the effectiveness of the combined use of temozolomide and an activator of an iron-dependent form of cell death. We will also test the safety of our approach in relation to healthy brain cells, which will potentially allow us to assess the rationality of further preclinical and then clinical trials in humans," said Tatiana Mishchenko.
The development of combined therapy methods and increasing the effectiveness of combined chemotherapy in oncology are urgent tasks. These approaches make it possible to achieve similar therapeutic results, but with less toxicity, or to increase the effectiveness of treatment for a larger number of patients, the head of the Department of Biochemistry told Izvestia. Academician T.T. Berezova RUDN University Vadim Pokrovsky.
"Currently, immunotherapeutic methods are actively being investigated, and the application of these approaches to brain tumors is of particular interest," the scientist said.
What scientists have done is the so—called sonotoxic effect (from the word sono — sound), when temozolomide was more effective at releasing reactive oxygen species during ultrasound irradiation, Mikhail Bolkov, researcher at the Institute for the Study of Aging at the Russian State Scientific and Clinical Center of the Russian National Research Medical University named after N.I. Pirogov, commented on the development.
— Scientists have tested the reaction In vivo and proved that this combination really enhances the destruction of tumor cell structures. As a result, temozolomide causes DNA disorders, and the simultaneous local destruction of glioblastoma cells enhances the immune response," the expert said.
— The idea of using a combination of different drugs that affect the tumor in different ways seems intuitive. The idea of using nanocarriers to treat brain tumors is not new, it has been around for more than a decade. However, it is premature to make any predictions, even if the safety of the approach for healthy brain cells is still being planned for testing, as follows from the comment of the project manager," said Stanislav Stragnov, head of the Laboratory for the Analysis of public health indicators and digitalization of healthcare at MIPT.
The results of the study, supported by a grant from the Russian Science Foundation (RSF), are published in Trends in Cancer.
Переведено сервисом «Яндекс Переводчик»







